Have You Heard of Salugenesis?
- Henry & Henry

- Nov 5, 2024
- 7 min read
Updated: Nov 8, 2024
I was surprised to receive an email from Doug Evans just recently about Salugenesis. He wasn't addressing me personally, he sends them out from the Sprouting Company to those of us who are fans of sprouting and get a buzz from his passion for sprouts! It was the subject matter that surprised me as it's something that recently captured my interest in a light-bulb-moment kind of way.
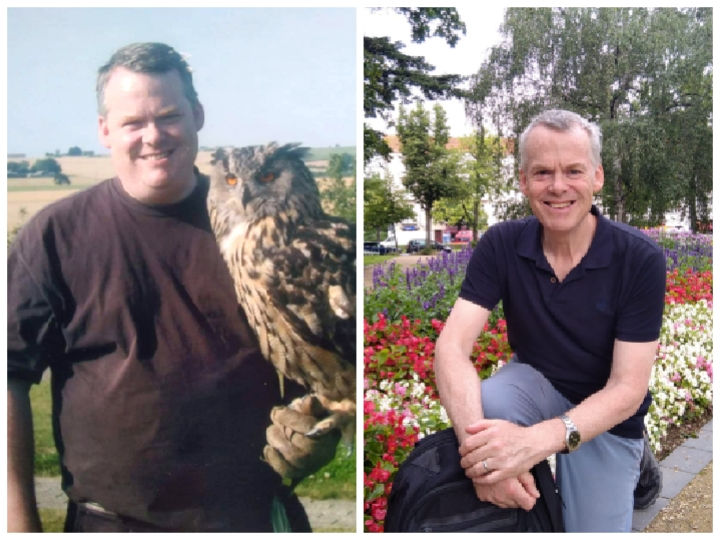
Salugenesis is a term coined by Dr Naviaux to refer to the body’s 3 stage process of recovery from injury, trauma, chronic stress or infection. But as the blog post from the Sprouting Company explains, this natural healing process sometimes gets stuck and chronic illness can ensue. I wrote about it, too, when I realised that it very probably applied to me. In my blog post I suggested that the multifaceted approach to supporting this healing process must emphasise the Vagus Nerve and I still maintain that it must. Why did I not know about this much sooner? Once again, although the information comes from science, we don’t tend to hear about it from the world of medicine (which probably answers my question!)
This extensive nerve, or more accurately, pair of nerves, wanders (hence the name ‘vagus’) from the brain to the intestines, reaching out to organs along its route and enabling communication from them to the brain and the other way too, although around 80% of the communication is from the body up to the brain. It thus has a role in cardiac health as a result of its relationship with the heart and in respiration resulting from its connection to the lungs. It links up with the liver, the kidneys, the pancreas, the spleen, the stomach as well as the large and small intestines and provides sensory feedback on all of them which then influences the instructions coming from the ‘command centre’ ie the brain, to the body.
It would be beyond the scope of both a blog post and of a non-scientist, me, to detail all of the functions of the Vagus Nerve in conjunction with each organ and more, because there is more!, but suffice to say the full information would constitute a very weighty tome. However, since sprouts are getting some of the focus in the blog post from the Sprouting Company (with whom I have no links, financial or otherwise), I will make reference to one. It’s the relationship of the Vagus Nerve and the organs of the digestive system.
We’re talking here about the two-way relationship known as the Gut Brain Axis. The Vagus Nerve becomes active when we’re in ‘rest and digest’ mode thus allowing digestion to proceed as it should as long as it is functioning properly. As with Naviaux’s observation about what causes cells to initiate their 3 stage recovery process, the same issues can impact the Vagus Nerve and leave it injured, inflamed or functioning sub-optimally. When this is the case, it can lead to low stomach acid and low enzyme production both of which contribute to poor digestion. Additionally, the Vagus Nerve stimulates the digestive tract muscles to enable peristalsis, ie the movement of food and waste through the gastrointestinal tract. A damaged nerve can therefore lead to constipation, diarrhoea, bloating and nausea. This seems to be spectacular enough but more is being discovered about the role of this nerve in the Gut-Brain-Axis of communication. It's now known that the Vagus Nerve can sense the metabolites produced by the gut microbiota, and inform the brain, thus influencing the production of neurotransmitters such as serotonin, melatonin and acetylcholine. In addition, this axis has been shown to modulate brain functions, such as emotional behaviour and our response to stress.¹ It’s becoming less surprising then that many of us with Chronic Fatigue, Long Covid, Fibromyalgia and other chronic conditions may experience symptoms such as brain fog, sleeplessness, low mood, anxiety. These conditions are frequently accompanied by gut dysbiosis² (an imbalance of the microorganisms in the gut) and thanks to the information superhighway between the gut and the brain, the unfavourable gut microbiota have an impact on the brain. It strikes me as imperative, therefore, to eat the foods that support good gut health AND work to heal the Vagus Nerve so that compromised digestion doesn’t thwart the efforts of optimal food choices! Can you imagine eating the best organic ‘healing’ foods only for them to make much less difference than you’d hoped for? Maybe you’ve already experienced it. If your Vagus Nerve needs to heal then both approaches could well be a good move. As this post is primarily about the Vagus Nerve, I’ll refrain from the temptation to extol the virtues of plant foods for providing pro- and prebiotics to restore good gut health, but if you’d like to immerse yourself in sprouting, we have a comprehensive guide to get you going.
So, how do you heal an inflamed or damaged Vagus Nerve? Before I leave the subject of food, it’s worth mentioning that a diet of whole foods emphasising nutrients such as magnesium, B group vitamins and anti-inflammatory phytochemicals is most supportive of nerve health. This brings us back to a diet of mostly or exclusively plant foods in their whole form. So while you’re healing your gut dysbiosis, if that applies to you, many of the same foods will nourish your nerves. How about that for convenience?!
But back to the Vagus Nerve. The good news is that there are many ways to stimulate the Vagus Nerve and I strongly recommend using any that you enjoy / can do / have access to. These include: massage, laughter, singing, humming, reflexology, acupuncture, meditation, mindfulness, cold water therapy and breathing. The list is not exhaustive and not all of them will be suitable. It’s worth mentioning that cold water therapy refers first and foremost to cold water on the head, face, neck, chest, upper back as doing so activates the diving response which is associated with parasympathetic nervous system activity (rest and digest mode) whereas body immersion is a stressor and thus puts us into sympathetic drive (fight / flight). Doing both, i.e. full body immersion, can be dangerous as it has the potential to cause fatal cardiac arrhythmia³. So for this one it makes sense to proceed with care and maybe graduated experimentation if it appeals to you.
Everything listed above is effectively an intervention, in other words, an activity that you undertake as a means to an end, in this case to stimulate the Vagus Nerve. But there is one that can be both an intervention and saboteur. I’m referring to breathing. You’ve probably heard that slow diaphragmatic breathing stimulates the Vagus Nerve and this is quite right, but what if your day-to-day, moment-by-moment breathing is dysfunctional as it is likely to be if you have any of the conditions referred to earlier?⁴ If this is the case, you can have the most magnificent massage, a burst of brilliant breathing, or a super singing session only for your respiratory pattern to undo all the good work shortly afterwards. Breathing must be retrained for successful progress. A number of the characteristics of dysfunctional breathing are listed on this page of our website. If any of these apply to you then there’s room for improvement and that’s great news because as your breathing returns to a more natural ‘normal’, you will start to experience improvements in your health.
I recommend a program of breathing retraining with an emphasis on slow, light breathing as a priority in order to reduce overbreathing. If this is not addressed, apart from the already-mentioned sabotage then the breathing exercise itself (the slow diaphragmatic breathing to stimulate the Vagus Nerve) can serve to perpetuate the overbreathing habit and maintain an over-sensitivity to carbon dioxide which in turn will keep you breathing a little bit too fast, too upper chest and possibly even through an open mouth even with the slightest exertion! Needless to say, you will assume ‘breathing’ doesn’t work.
Human beings don’t feel as rewarded by removal or scaling back as they do by making actual gains and this is where the really good news comes in. As you’re working to undo the breathing patterns that are holding you back, the newer patterns, slower, lighter, deeper (ie to the lower lobes of the lungs) breathing presents you with subtle, and sometimes not so subtle gifts. Don’t be surprised to feel a little bit better, feel a little less anxious maybe, perhaps sleep a little better, notice a little more energy more often than you have been doing or to feel more resilient and capable. And there’s more. Working on your Vagus Nerve isn’t just a temporary thing. In the same way that a muscle gets toned with repeated exercise, so can vagal tone increase with relevant practice. So if, for example, you experience disturbed sleep relating to your condition and current physiology rather than worrying thoughts, practise slow, light breathing because even if it doesn’t get you back to sleep (which it might!) you’ll be working on your vagal tone. On the subject of worry, breathing can help with this, too but the Emergency Exercise may be the better option in this case at least to bring initial calm. There’s a video of me demonstrating this on our Breathing Space.
And finally, if this speaks to you as a result of nervous system dysregulation and or a fatigue-related condition, do work on your breathing as if it were a prescription. If going it alone is too much, then maybe consider partnering with someone who can help. You can always book a free 20 minute Zoom call with me if you’d like to discuss the possibility of working with me. Whatever you decide to do, I wish you well. Believe that feeling better is possible.
~Annette Henry

¹Almeida C, Oliveira R, Soares R, Barata P. Influence of gut microbiota dysbiosis on brain function: a systematic review. Porto Biomed J. 2020 Mar 17;5(2):1-8. doi: 10.1097/j.pbj.0000000000000059. PMID: 33299942; PMCID: PMC7722401.
²Wang, JH., Choi, Y., Lee, JS. et al. Clinical evidence of the link between gut microbiome and myalgic encephalomyelitis/chronic fatigue syndrome: a retrospective review. Eur J Med Res 29, 148 (2024). https://doi.org/10.1186/s40001-024-01747-1
³Shattock MJ, Tipton MJ. 'Autonomic conflict': a different way to die during cold water immersion? J Physiol. 2012 Jul 15;590(14):3219-30. doi: 10.1113/jphysiol.2012.229864. Epub 2012 Apr 30. PMID: 22547634; PMCID: PMC3459038.
⁴Ravindran M, Adewuyi O, Zheng Y, Rayhan RU, Le U, Timbol C, Merck S, Esteitie R, Read C, Cooney M, Baraniuk J. Dyspnea in Chronic Fatigue Syndrome (CFS): comparison of two prospective cross-sectional studies. Glob J Health Sci. 2012 Dec 12;5(2):94-110. doi: 10.5539/gjhs.v5n2p94. PMID: 23445698; PMCID: PMC4209305.

)_20230830_134131_0000.png)


Comments